Healthcare File Sharing: A Complete Guide to Secure and Compliant Data Exchange
Healthcare data breaches affected over 116 million individuals in 2024 alone. Over 112 million individuals were affected by healthcare data breaches in 2023, highlighting the growing scale of this issue. These breaches have a significant impact on affected individuals, whose sensitive medical information may be exposed or misused. Each incident represents more than statistics—it’s patient trust broken, regulatory violations incurred, and organizational reputations damaged. The U.S. Department of Health and Human Services (HHS) enforces HIPAA regulations and investigates breaches that may infringe on civil rights, holding organizations accountable for protecting personal health information. For healthcare organizations navigating this landscape, secure file sharing isn’t optional anymore. It’s the foundation that makes modern patient care possible while keeping sensitive information protected.
Healthcare file sharing enables the secure exchange of protected health information between healthcare providers, patients, and business associates. This includes everything from electronic health records and medical imaging to lab results and billing documentation. Covered entities, as defined by HIPAA, are required to implement safeguards to protect electronic protected health information (ePHI), and each covered entity must assess risks and take appropriate measures to ensure compliance and data protection. The challenge lies in balancing accessibility for care teams with the stringent security requirements that protect patient privacy and ensure regulatory compliance. Encrypting data and ensuring data protection are essential for meeting HIPAA requirements in secure file sharing. Maintaining HIPAA compliance requires a thorough understanding of both technological and administrative safeguards, including preventing unauthorized access and implementing measures to safeguard data according to regulatory standards. Robust security should provide strong protection, following standards set by the National Institute of Standards and Technology (NIST). Secure file sharing also supports operational efficiency and leverages information systems to streamline healthcare workflows. In addition to healthcare, human services organizations must also ensure secure file sharing to protect sensitive client data. Protecting ePHI and ensuring secure data storage are critical for maintaining the confidentiality and integrity of sensitive information. Organizations can choose from a range of solutions, including HIPAA compliant services, to meet their security and compliance needs.
What is Healthcare File Sharing and Why It Matters
Healthcare file sharing forms the digital backbone of modern medical practice. When a radiologist sends CT scan images to an emergency physician at 2 AM, when lab results flow automatically into a patient’s electronic health record, or when specialists collaborate on treatment plans across different hospital systems—that’s healthcare file sharing in action. Platforms like Dropbox Business, which is HIPAA-compliant and offers critical protections such as Business Associate Agreements (BAAs), exemplify the secure solutions available for these vital exchanges. These platforms often include additional features such as activity tracking, device management, and data leak prevention, which enhance security and provide comprehensive protection beyond basic encryption. Google Drive is HIPAA compliant only when used with Google Workspace and requires a signed BAA, making it another viable option for secure file sharing. Box’s Enterprise Plan includes essential security features like two-factor authentication and customizable access controls for HIPAA compliance, further expanding the range of secure file-sharing solutions. FileCloud offers both self-hosted and cloud-hosted HIPAA-compliant file sharing with strong data security features, providing additional flexibility for healthcare organizations.
The stakes couldn’t be higher. A single compliance violation can trigger HIPAA fines ranging from $137 to $2 million per incident. HIPAA compliance violations can also lead to civil monetary penalties ranging from $137 to $68,928 per infraction, depending on the severity and circumstances. Non-compliance can lead to significant fines, with maximum penalties reaching $1.5 million per violation. In the event of a data breach or security violation, organizations may also face an OCR investigation to determine whether HIPAA security requirements were met and proper data protection measures were enforced. Organizations need to ensure compliance with regulations to avoid hefty fines and reputational damage. More importantly, secure file sharing directly impacts patient outcomes by enabling faster diagnoses, seamless care coordination, and smoother transitions between healthcare providers and care settings.
Modern healthcare workflows demand real-time collaboration. Emergency departments need instant access to patient histories from primary care providers. Specialists require high-resolution imaging files that can exceed several gigabytes. Insurance companies process thousands of claims daily, each containing sensitive patient data. All of these exchanges must happen securely, efficiently, and in compliance with federal regulations. Health care providers rely on these secure file sharing platforms to transmit protected health information (PHI) while maintaining compliance. Each healthcare provider involved in the exchange of PHI must ensure that legally binding agreements, such as Business Associate Agreements (BAAs), are in place to meet HIPAA requirements.
The shift toward cloud-based, hipaa compliant solutions has transformed how healthcare entities handle data. These platforms offer real-time access across multiple devices, streamlined workflows, and disaster recovery capabilities that traditional file sharing methods simply can’t match.
HIPAA Requirements for Healthcare File Sharing
The Health Insurance Portability and Accountability Act sets the regulatory framework that governs all healthcare file sharing activities. The HIPAA Privacy Rule is a key component, establishing standards for protecting personally identifiable health information and ensuring compliance with regulatory standards. The Omnibus Rule, introduced in 2013, expanded HIPAA compliance requirements to include business associates, ensuring that all entities handling protected health information adhere to the same standards. HIPAA compliance isn’t just about avoiding fines—it’s about implementing a comprehensive security strategy that protects patient information at every step of the data exchange process.
Healthcare organizations must establish three layers of protection: administrative safeguards, physical safeguards, and technical safeguards. Each layer addresses different aspects of data security and works together to create a robust defense against unauthorized access and data breaches. The HIPAA Security Rule requires implementing administrative, physical, and technical safeguards for ePHI.
Technical Safeguards for Secure File Sharing
Technical safeguards form the technological foundation of secure healthcare file sharing. End-to-end encryption using transport layer security (TLS) 1.2 or higher protects data in transit, ensuring that files remain encrypted as they move between systems. This means even if network traffic is intercepted, the protected health information remains unreadable to unauthorized parties. HIPAA requires encryption of protected health information (PHI) of patients when the data is at rest, further emphasizing the importance of robust encryption protocols. Data is considered 'at rest' when it is stored on devices like servers and hard drives. HIPAA describes encryption as an 'addressable' requirement, meaning it is often necessary for compliance.
Multi-factor authentication adds a critical verification layer. Healthcare professionals must provide multiple forms of identification—typically something they know (password), something they have (mobile device), or something they are (biometric data)—before accessing sensitive files. This approach significantly reduces the risk of unauthorized access, even when login credentials are compromised. Additionally, administrators can set custom access controls in file-sharing platforms to restrict data access, ensuring that only authorized personnel can view or modify sensitive information.
Session timeouts and automatic logouts prevent unauthorized access from unattended devices. In busy healthcare settings where professionals move quickly between patients and workstations, these features ensure that sensitive data doesn’t remain accessible on abandoned screens.
File integrity monitoring detects unauthorized modifications or tampering attempts in real-time. This capability is essential for maintaining the accuracy of medical records and identifying potential security breaches before they escalate.
Administrative Safeguards for File Sharing Compliance
Administrative safeguards establish the human and procedural elements of data protection. Healthcare organizations must designate security officers with clear oversight responsibilities for all file sharing policies and procedures. These professionals ensure that security measures keep pace with evolving threats and regulatory requirements.
Regular employee training addresses the human element of data security. Healthcare professionals need to understand not just how to use secure file sharing systems, but why these protections matter. Training programs should cover current HIPAA requirements, emerging threats, and the specific procedures their organization has implemented.
Risk assessments identify vulnerabilities in file sharing workflows and technical systems. These evaluations should examine both obvious weak points—like outdated software or inadequate access controls—and subtle risks that emerge from how staff actually use file sharing tools in their daily work. Business associates account for over 54% of total data breaches affecting patients, highlighting the importance of evaluating third-party risks during these assessments.
Incident response procedures ensure that data breaches or security violations receive prompt attention. Clear protocols help organizations contain breaches quickly, investigate their scope, and report incidents to the appropriate authorities as required by HIPAA regulations.
Advanced Encryption for Secure Data Exchange
Advanced encryption is the cornerstone of HIPAA compliant file sharing, providing healthcare organizations with the tools needed to safeguard sensitive data during every stage of exchange. By leveraging robust encryption protocols such as Transport Layer Security (TLS) and Advanced Encryption Standard (AES), healthcare providers can ensure that electronic health records, protected health information (PHI), and other sensitive data remain confidential and protected from unauthorized access. End-to-end encryption is especially vital, as it secures data in transit between systems and devices, making it unreadable to anyone except authorized recipients.
For healthcare professionals, advanced encryption enables secure file transfer of large files, including medical records and lab results, without compromising data integrity or patient privacy. This is particularly important when sharing information across different healthcare organizations or with external partners. By implementing strong encryption measures, healthcare entities can significantly reduce the risk of data breaches, maintain compliance with HIPAA regulations, and build trust with patients who rely on the security of their personal health information. Ultimately, advanced encryption not only protects sensitive information but also supports efficient, HIPAA compliant file sharing that is essential for modern patient care.
Protecting Data in Transit
Ensuring the security of data in transit is a fundamental requirement for HIPAA compliance, as sensitive information is frequently exchanged between healthcare organizations, providers, and business associates. To protect data as it moves across networks, healthcare entities must utilize secure file transfer protocols such as Secure File Transfer Protocol (SFTP) and Hypertext Transfer Protocol Secure (HTTPS). These protocols employ encryption technologies like TLS to shield sensitive data from interception or tampering during transmission.
In addition to encryption, implementing strict access controls is essential. Two-factor authentication and robust authorization processes help verify the identity of users and ensure that only authorized parties can initiate or receive file transfers. By combining secure file transfer protocols with strong access controls, healthcare providers can effectively prevent data breaches, safeguard sensitive information, and comply with HIPAA regulations. Protecting data in transit not only maintains the confidentiality and integrity of patient information but also reinforces the trust that patients place in their healthcare providers and organizations.
Data at Rest Security
Securing data at rest is a critical aspect of protecting sensitive information stored on servers, laptops, and mobile devices within healthcare organizations. To achieve HIPAA compliance, healthcare providers must implement comprehensive encryption strategies, such as full-disk encryption and file-level encryption, which ensure that data remains protected even if a device is lost or stolen. These measures are particularly important for mobile devices, which are more susceptible to theft or unauthorized access.
Beyond encryption, healthcare entities should enforce strict access controls, including authentication and authorization protocols, to limit data access to only those individuals who are explicitly permitted. Regular security audits and risk assessments are also vital, as they help identify potential vulnerabilities and ensure that security measures remain effective and up to date with HIPAA regulations. By prioritizing data at rest security, healthcare providers can prevent data breaches, protect patient information, and demonstrate a strong commitment to maintaining HIPAA compliance and patient trust.
Business Associate Agreement Requirements
A Business Associate Agreement (BAA) is an essential element of HIPAA compliance, defining the responsibilities and expectations for any business associate that handles protected health information (PHI) on behalf of a healthcare organization. Healthcare providers must enter into a BAA with all contractors, vendors, and subcontractors who may access, store, or transmit PHI. The agreement should clearly outline the terms for handling, storing, and transmitting PHI, as well as the security measures—such as encryption and access controls—that business associates are required to implement.
By establishing a comprehensive BAA, healthcare organizations ensure that their business associates adhere to HIPAA regulations and maintain the same high standards for data protection and regulatory compliance. Regularly reviewing and updating BAAs is also crucial, as it allows organizations to address changes in business relationships or regulatory requirements. Ultimately, a well-crafted BAA helps healthcare providers protect patient information, reduce the risk of non-compliance, and foster a culture of accountability and security throughout the healthcare ecosystem.
Types of Files Shared in Healthcare Settings
Healthcare file sharing encompasses a diverse range of file types, each presenting unique challenges for secure transmission and storage. Understanding these different categories helps organizations implement appropriate security measures and choose platforms capable of handling their specific needs.
Electronic health records represent the most comprehensive category of shared files. These documents contain complete patient medical histories, diagnoses, treatment plans, and ongoing care notes. EHRs require sophisticated access controls since different healthcare providers need different levels of information depending on their role in patient care.
Medical imaging files including X-rays, MRIs, CT scans, and ultrasounds present particular challenges due to their large file sizes. A single high-resolution MRI study can exceed several gigabytes, requiring specialized transfer solutions that can handle these massive datasets efficiently while maintaining security standards.
Laboratory results and pathology reports facilitate real-time clinical decision-making. These files often contain time-sensitive information that directly impacts patient treatment decisions, making secure and rapid transmission essential for quality care.
Insurance claims and billing documentation support the financial operations of healthcare organizations. While these files may seem less critical than clinical data, they contain protected health information that requires the same level of security as medical records.
Research data and clinical trial information represent an increasingly important category as healthcare organizations participate in medical studies and drug development programs. These files often contain experimental protocols and patient participant data that demand strict access controls and audit trails.
Best Practices for Secure Healthcare File Sharing
Effective healthcare file sharing begins with implementing minimum necessary standards. This principle ensures that only the protected health information required for specific healthcare purposes gets shared, reducing exposure and limiting potential damage from any security incidents.
Selecting the right platform makes all other security measures possible. Organizations should choose secure file transfer solutions specifically designed for HIPAA compliance, with built-in audit trails, granular access controls, and business associate agreements that clearly define security responsibilities.
Setting file expiration dates and download limits helps control how long sensitive data remains accessible and prevents unauthorized data accumulation. These features are particularly important when sharing files with external partners or temporary consultants who should lose access when their involvement ends.
Remote wipe capabilities provide essential protection for files accessed on mobile devices or laptops. If a device is lost or stolen, administrators can remotely delete sensitive files before unauthorized parties can access them. Remote wipe features enhance security by ensuring that sensitive data does not remain vulnerable on compromised devices. This capability is crucial in healthcare settings where staff frequently work with portable devices. Remote wipe features can enhance security for file-sharing services by allowing businesses to erase data from lost or stolen devices.
Regular software updates address known security vulnerabilities and ensure that file sharing systems maintain their protective capabilities. Organizations should establish procedures for testing and deploying updates promptly while minimizing disruption to clinical workflows.
Mobile Device Security for Healthcare File Sharing
Mobile devices enable healthcare providers to access patient information at the bedside, in remote clinics, or while on-call, but they also introduce significant security risks. Proper mobile device management balances accessibility with protection of sensitive data.
Device encryption and passcode protection form the foundation of mobile security. All devices that access healthcare files must encrypt data at rest and require strong authentication to unlock. This protection ensures that lost or stolen devices don’t automatically compromise patient information.
Mobile device management solutions give organizations centralized control over which applications can access protected health information and how that data gets stored and transmitted. MDM platforms can enforce security policies, monitor compliance, and remotely manage devices across large healthcare organizations.
Containerization separates work and personal data on employee-owned devices, addressing the growing trend of bring-your-own-device policies in healthcare settings. This approach allows staff to use personal smartphones and tablets for work while ensuring that patient data remains isolated from personal applications and accounts.
Disabling cloud synchronization features prevents the unintentional storage of protected health information on unsecured consumer platforms. Many mobile devices automatically sync files to services like iCloud or Google Drive, which lack the security safeguards required for healthcare data.
Common Healthcare File Sharing Challenges and Solutions
Healthcare organizations face several persistent challenges when implementing secure file sharing systems. Understanding these obstacles and their solutions helps organizations prepare for successful deployments and ongoing operations.
Large file sizes from medical imaging create bandwidth and storage challenges that traditional email systems simply can’t handle. Modern managed file transfer solutions address this issue with optimized compression algorithms, resumable transfers, and dedicated high-speed connections that can efficiently move multi-gigabyte datasets.
Legacy systems integration remains problematic for many healthcare organizations operating with older electronic health record systems or specialized medical equipment that generates proprietary file formats. Modern platforms address these challenges through robust APIs and support for standardized healthcare data formats that bridge gaps between different systems.
Staff resistance to new technologies often emerges when organizations introduce new file sharing platforms. Healthcare professionals are busy, and learning new systems can feel like an additional burden. Comprehensive training programs and intuitive user interfaces help overcome this resistance by demonstrating clear benefits and minimizing learning curves.
Cost constraints frequently limit organizations’ ability to implement comprehensive secure file sharing solutions. Scalable pricing models that grow with organizational needs help address this challenge by avoiding large upfront investments while providing room for expansion as file volumes and user bases increase.
Interoperability between different healthcare systems has long been a significant hurdle. The adoption of Fast Healthcare Interoperability Resources (FHIR) standards and other widely supported data formats is helping to create smoother exchanges between diverse systems and organizations.
Choosing the Right Healthcare File Sharing Solution
Selecting an appropriate healthcare file sharing platform requires careful evaluation of several critical factors. The decision impacts not just current operations but also long-term scalability, compliance posture, and overall security effectiveness. OneDrive for Business includes user activity logging to help maintain compliance with HIPAA requirements, making it a viable option for organizations seeking secure and compliant file-sharing solutions. Kiteworks is designed for secure communications and meets HIPAA requirements for secure data transfers, offering another robust option for healthcare organizations.
Vendor HIPAA compliance represents the most fundamental consideration. Organizations should look for providers with current compliance certifications, regular SOC 2 audits, and demonstrated experience serving the healthcare industry. A business associate agreement should clearly define security responsibilities and liability allocation.
Comprehensive audit logging and reporting capabilities ensure ongoing compliance visibility. Healthcare organizations need detailed records of who accessed which files, when transfers occurred, and what actions users performed. These audit trails are essential for compliance monitoring and incident investigation.
Integration with existing healthcare applications determines how smoothly new file sharing systems will fit into current workflows. Platforms should offer robust connectivity with popular electronic health record systems like Epic, Cerner, and athenahealth, as well as practice management software and other clinical applications.
Scalability considerations become critical as organizations grow or experience seasonal variations in file sharing volumes. Solutions should handle increasing numbers of users, larger file sizes, and expanded geographic distribution without requiring major infrastructure changes or cost increases.
Pricing models deserve careful scrutiny beyond basic per-user costs. Organizations should examine storage limits, bandwidth charges, premium feature add-ons, and support tier pricing to understand total cost of ownership over time.
Key Features to Look for in Healthcare File Sharing Platforms
An effective healthcare file sharing platform must deliver specific capabilities that address the unique requirements of medical environments. These features work together to create a comprehensive solution that protects patient data while enabling efficient clinical workflows.
HIPAA-compliant infrastructure forms the foundation, with data centers designed specifically to meet healthcare security standards. This includes physical security measures, environmental controls, and access management protocols that protect servers and storage systems housing sensitive medical information.
User-friendly interfaces reduce training requirements and technological barriers for busy healthcare staff. The platform should feel intuitive to medical professionals who may not have extensive technical backgrounds but need to access and share files quickly and efficiently during patient care.
Cross-platform compatibility ensures that healthcare providers can access files regardless of their preferred devices or operating systems. Support for Windows, Mac OS, iOS, Android, and web browsers enables seamless collaboration across diverse technology environments.
Version control maintains accurate record keeping by tracking changes to shared files over time. This capability is essential for medical records where accuracy is critical and regulatory requirements mandate documentation of all modifications to patient information. The NIST Special Publication 800-111 provides guidelines for encryption technologies to secure data at rest, ensuring that stored information remains protected against unauthorized access or tampering.
Advanced encryption protects data both at rest and during transmission, using industry-standard protocols that meet or exceed HIPAA security rule requirements. End-to-end encryption ensures that files remain protected throughout their entire lifecycle, from creation to final deletion. ShareFile uses 256-bit AES encryption to protect data both at rest and in transit, ensuring HIPAA compliance and providing a robust solution for secure file sharing.
Future of Healthcare File Sharing
The healthcare file sharing landscape continues evolving rapidly, driven by technological advances and changing regulatory requirements. Organizations that understand these trends can position themselves to take advantage of emerging capabilities while maintaining strong security postures.
Artificial intelligence integration promises to automate many aspects of data classification and security policy enforcement. AI systems can automatically identify protected health information in shared files, flag content that requires special handling, and ensure compliance with organizational security policies without manual intervention.
Blockchain technology offers the potential for creating immutable audit trails that enhance data integrity verification. This approach could provide unprecedented transparency and accountability in healthcare file sharing, making it nearly impossible to alter or delete evidence of data access and transmission.
Zero-trust security models represent a fundamental shift from traditional network-based security approaches. These frameworks require continuous authentication and authorization for every file access, regardless of network location or user credentials, providing more granular control over sensitive information.
Cloud-native solutions continue to gain adoption, offering reduced infrastructure overhead and greater scalability compared to on-premises systems. These platforms can automatically scale to handle varying workloads while providing built-in disaster recovery and business continuity capabilities.
Enhanced patient portals will give patients more direct control over their health information, enabling secure file sharing between patients and healthcare providers, researchers, and family caregivers. This trend toward patient-controlled data sharing represents a significant shift in how healthcare information flows through the system.
The increasing frequency and sophistication of data breaches in the healthcare industry underscore the critical importance of robust file sharing security. Organizations that invest in comprehensive solutions today will be better positioned to protect patient information, maintain regulatory compliance, and preserve the trust that forms the foundation of effective healthcare delivery.
Healthcare file sharing technology will continue advancing, but the fundamental principles of protecting patient privacy, ensuring data integrity, and maintaining regulatory compliance will remain constant. Organizations that focus on these core objectives while staying current with technological developments will successfully navigate the complex landscape of secure healthcare data exchange.
The path forward requires ongoing vigilance, regular assessment of security practices, and willingness to adapt as new threats and opportunities emerge. By implementing strong foundational practices and remaining alert to changing requirements, healthcare organizations can harness the power of secure file sharing to improve patient outcomes while safeguarding the sensitive information entrusted to their care.
Frequently Asked Questions (FAQ) About Healthcare File Sharing
What is healthcare file sharing?
Healthcare file sharing refers to the secure exchange of protected health information (PHI) and other sensitive medical data between healthcare providers, patients, business associates, and healthcare organizations. It involves using HIPAA-compliant platforms and protocols to ensure data privacy and regulatory compliance.
Why is HIPAA compliance important in healthcare file sharing?
HIPAA compliance is critical because it mandates the protection of electronic protected health information (ePHI). Non-compliance can lead to severe penalties, including hefty fines and reputational damage. Using HIPAA-compliant file sharing solutions safeguards patient data and ensures adherence to regulatory standards.
What types of files are commonly shared in healthcare settings?
Commonly shared healthcare files include electronic health records (EHRs), medical imaging (X-rays, MRIs, CT scans), lab results, billing and insurance claims, and research data. Each type requires secure handling to maintain patient privacy and data integrity.
What security measures are essential for HIPAA-compliant file sharing?
Key security measures include advanced encryption (AES-256) for data at rest and in transit, access controls such as two-factor authentication, audit trails to monitor file access, session timeouts, remote wipe capabilities for lost or stolen devices, and strict administrative safeguards like employee training and risk assessments.
What is a Business Associate Agreement (BAA) and why is it necessary?
A Business Associate Agreement is a legally binding contract between a healthcare provider and a vendor or business associate who handles PHI. It ensures that both parties are responsible for maintaining HIPAA compliance and protecting sensitive patient data during storage, transmission, or processing.
How can healthcare organizations protect data in transit?
Healthcare organizations protect data in transit by using secure protocols like Transport Layer Security (TLS) and Secure File Transfer Protocol (SFTP). These encrypt data during transmission, preventing unauthorized interception or tampering.
What is the difference between data at rest and data in transit?
Data at rest refers to information stored on devices like servers, hard drives, or mobile devices, while data in transit is data actively moving between systems or users. Both states require strong encryption and security measures to comply with HIPAA regulations.
Are cloud-based file sharing solutions HIPAA compliant?
Cloud-based solutions can be HIPAA compliant if they implement required safeguards, sign a Business Associate Agreement, and follow HIPAA security rules. Many platforms, such as Dropbox Business, Google Workspace, and FileCloud, offer HIPAA-compliant cloud storage and file sharing.
How do remote wipe features enhance healthcare file sharing security?
Remote wipe allows administrators to erase sensitive data from lost or stolen devices remotely, preventing unauthorized access to protected health information. This feature is essential for mobile devices frequently used in healthcare settings.
What role do audit trails play in healthcare file sharing?
Audit trails provide detailed logs of who accessed files, when, and what actions were taken. They are crucial for maintaining regulatory compliance, detecting unauthorized access, and facilitating investigations in case of data breaches.
How can healthcare providers ensure operational efficiency while maintaining security?
By choosing HIPAA-compliant file sharing platforms with user-friendly interfaces, cross-platform compatibility, and integration with existing healthcare applications, providers can streamline workflows without compromising data security or patient privacy.
What are the consequences of HIPAA non-compliance in file sharing?
Consequences include civil and criminal penalties, fines up to $1.5 million per violation, legal actions, loss of patient trust, and damage to organizational reputation. Non-compliance also increases the risk of data breaches and associated costs.
How often should healthcare organizations conduct risk assessments for file sharing?
Regular risk assessments should be conducted at least annually or whenever significant changes occur in technology, workflows, or regulatory requirements. These assessments help identify vulnerabilities and ensure ongoing compliance with HIPAA.
Can personal devices be used for healthcare file sharing?
Personal devices can be used if they comply with security policies, including encryption, strong authentication, and mobile device management. Containerization and disabling cloud sync features help isolate and protect sensitive healthcare data on personal devices.
What features should healthcare organizations look for in a file sharing platform?
Important features include HIPAA compliance certification, advanced encryption, two-factor authentication, audit trails, remote wipe capabilities, user access controls, file expiration settings, integration with healthcare systems, and scalability to handle large files and user volumes.
How does encryption protect patient privacy in healthcare file sharing?
Encryption transforms sensitive data into unreadable formats that only authorized parties can decrypt. This protects patient privacy by preventing unauthorized access during storage and transmission, ensuring data integrity and compliance with HIPAA security standards.
What is the role of the National Institute of Standards and Technology (NIST) in healthcare file sharing security?
NIST provides guidelines and standards for encryption and security protocols that healthcare organizations must follow to comply with HIPAA. Their recommendations help ensure that data protection measures are robust and effective against evolving cyber threats.
How can healthcare organizations handle large medical files securely?
Using managed file transfer (MFT) solutions optimized for large files, such as medical imaging, enables secure, efficient transmission without compromising compliance. Features like resumable transfers, compression, and dedicated bandwidth help manage large data volumes.
Are there specific regulations for sharing patient data with third-party vendors?
Yes, HIPAA requires healthcare organizations to have Business Associate Agreements with third-party vendors who access PHI. These agreements mandate compliance with HIPAA security and privacy rules to safeguard patient data.
How do healthcare file sharing solutions support patient care?
Secure healthcare file sharing enables timely access to medical records, lab results, and imaging, facilitating faster diagnoses, coordinated treatment plans, and improved communication between providers, ultimately enhancing patient outcomes.
What steps should be taken after a data breach involving healthcare file sharing?
Organizations should follow incident response procedures, including containment, investigation, notification to affected parties and regulatory bodies, remediation of vulnerabilities, and review of security policies to prevent future breaches.
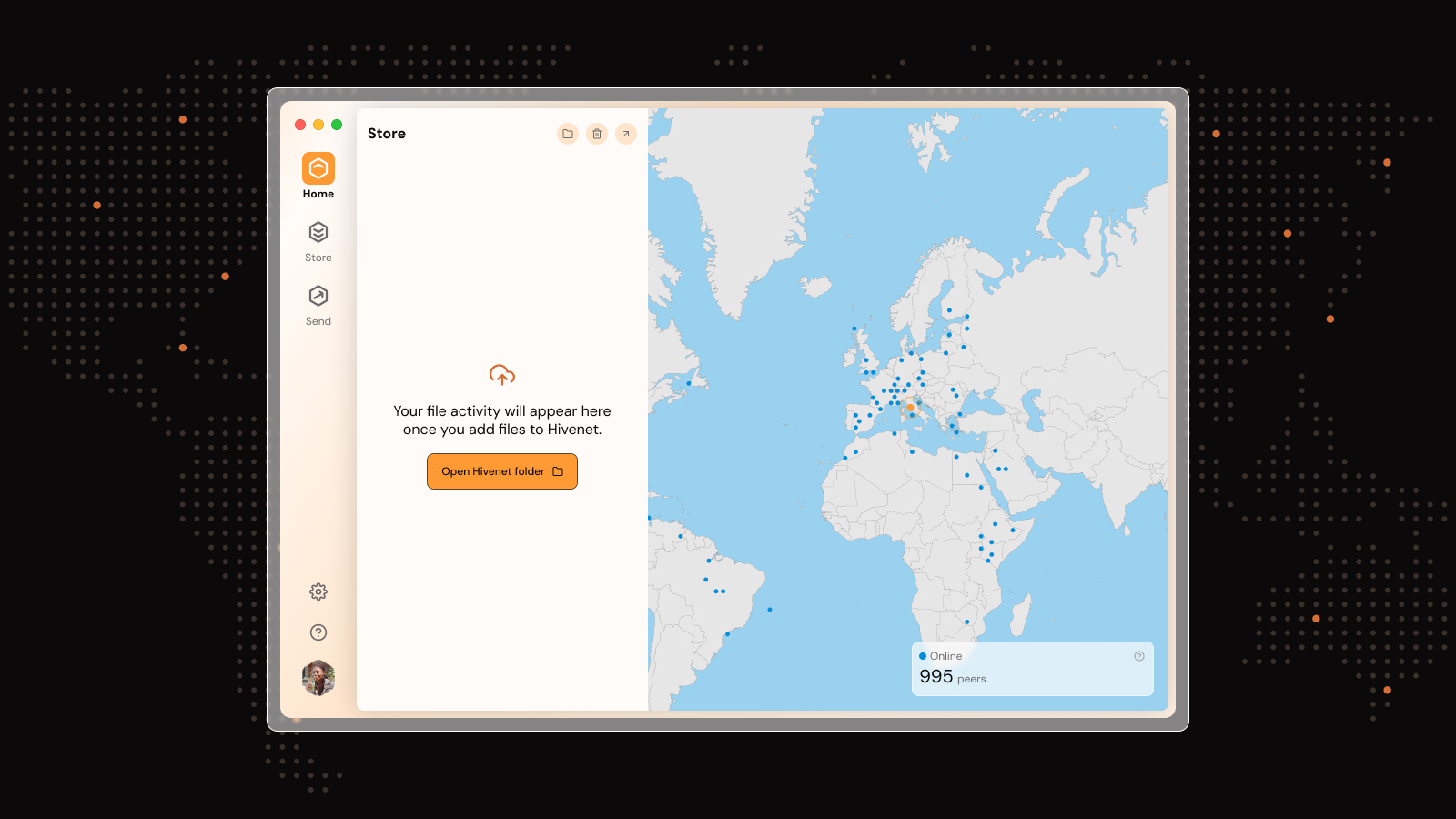
Liked this article? You'll love Hivenet



You scrolled this far. Might as well join us.
Secure, affordable, and sustainable cloud services—powered by people, not data centers.